A few weeks ago I had a patient in the ICU who had been intubated and placed on a ventilator. This patient had critical aortic stenosis and was placed on a ventilator following an attempted right internal jugular line placement that resulted in a massive right hemothorax. On the day that I was in the ICU the physician and primary RN decided that they would taper the patient down off the Sublimaze (fentanyl) and Versed (midazolam) being used for analgesia and sedation. The team’s ultimate goal was to see if the patient was ready to be extubated. In addition, the patient was placed on CPAP as a trial. In this particular case it was very important that the patient be monitored for any signs of agitation or distress due to the fact that increased stress would activate the sympathetic nervous system and increase the workload on the heart. Due to the severe aortic stenosis and compromised cardiac function, an increase in workload would be poorly tolerated by the patient. By noon the patient started to respond to stimulation. The patient would open his eyes in response to voices and became agitated during suctioning and turning. The increased heart rate that accompanied the agitation required that the Sublimaze and Versed be initiated once again. Ultimately, the respiratory therapist, nurse, and physician agreed that based on the trial CPAP and spontaneous awakening trial, the patient was not ready to be extubated. Ventilation and sedation are often a necessary treatment for a person with severely compromised cardio-pulmonary function. Nonetheless, these treatments have to be used judiciously with constant reappraisal of the situation in order to minimize the potential short- and long-term consequences of ICU-acquired delirium and weakness. During my next ICU clinical I look forward to investigating the procedures and protocols that are instituted in the hospital units.
Category Archives: Goleta420
Sedation Vacation
Sedation Vacation
Sedation vacation is a term used in the critical care field and refers to patients that are sedated and on a ventilator . The sedative is titrated down in order to perform Neuro checks and assess for the possibility of extubating. The sedation vacation is necessary to reduce ventilator acquired pneumonia, delirium from the sedatives and a shorten ICU stays. This however does not mean that all the patients in the critical care units receive a sedation vacations. The patient has to meet certain criteria. Criteria like being Hemodynamically stable, shows no agitation on current sedative regiment, Fio2 is less than 50% and Peep is less than 10%, the sedation is not used to control status epilepticus or symptoms of alcohol withdrawal. Patient must also not be on a Blakemore tube for the control of bleeding varices. If a patient does not meet these criteria then the patient is not eligible yet for a sedation vacation. But as with all and any medical procedure there is a Policy for that which is basically describing how and when to perform this sedation vacation. The following is a Policy and Procedure form The Jefferson University Hospital
NURSING CRITICAL CARE PROCEDURES
Purpose Daily lightening of sedation, “Sedation Vacations”, and assessing the patient’s readiness to extubate is an integral part of the Ventilator Bundle and has been correlated with reduction in the rate of ventilator-acquired pneumonia. This procedure is generally initiated after 48 hours of continuous sedation. Kress et al. demonstrated that daily interruption of continuous sedation decreased the length of time patients spend on the ventilator and in the ICU and diminished the number of diagnostic tests performed to evaluate why a patient was not waking up once sedatives had been discontinued. This protocol involves daily 50% dose reduction, and furthermore decreasing the sedation of the continuous drug infusion (including opiates) and monitoring the patient until he or she starts to show signs of awakening or agitation. At this time the patient is assessed for readiness to wean. The patient can also be assessed neurologically at this time. The continuous sedation infusions can be titrated at the discretion of the bedside nurse to achieve a Ramsay sedation score of 2 to 3. In comparison with routine management, the daily cessation of drug infusions significantly reduced time on the ventilator in the ICU and provided a valuable window of opportunity for assessment of the patient’s neurologic function.
Documentation Nursing: 1. Critical Care Flowsheet/JeffChart – document wean attempt, ventilator settings, and success or failure of procedure. Document patient’s response to SBT. 2. ABG results 3. Document neurological assessment and response to decreased sedation.
Respiratory: 1. Respiratory Flowsheet – document wean ventilator settings and response to attempt to wean. 2. Document assessment findings and patient response that indicated success or failure of wean.
References
Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. New England Journal of Medicine. May 18 2000;342(20):1471-1477.
|
|||||||||||||||||||||||||||||||||||||||||
References
Jefferson University Hospital Sedation Vacation protocal retrieved from
http://hospitals.jefferson.edu/
Strategies for Sedation Vacation in the MICU retrieved from
http://www.aacn.org/wd/ntispeakermats/PosterPresentations/00042670/00042670.swf
Pacemakers & Cellphones: Keep Your Distance
It seems like everyone and their brother has a smart phone of some sort these days or at least is exposed to someone who has one. And for patients with pacemakers, this could be a dangerous combination. I look at the medical news on my favorite science-oriented website regularly and a new study from the European Society of Cardiology found that those who have pacemakers should keep their distance from cell phones to avoid unwanted painful shocks or frightening pauses in the function of their device. The study was presented in June to the joint meeting of the European Heart Rhythm Association and the European Society of Cardiology by one of the main authors, Dr. Carsten Lennerz, a cardiology resident in Germany.
Although it does not happen all the time, pacemakers can sometimes mistakenly pick up electromagnetic interference from smartphones and treat them like a cardiac signal, which can cause them to stop working for a brief period of time, according to Lennerz. He recommends that patients should hold their phone on the ear opposite to their pacemaker when talking and not place the phone in a pocket directly above the pacemaker just to be safe.
The authors added that another area of concern for patients with pacemakers is when they are under high voltage power lines. Although is ok for them to walk under power lines, the authors recommend that they do not spend extra time under the power lines, as high electric fields can also tamper with the pacemaker’s normal functioning.
I found it interesting and worrisome that the authors noted that pacemakers themselves do not come with any warnings about these possible problems. My uncle has a pacemaker that has saved his life and next time I see him walking around with his cell phone in his pocket as he often does, I will be sure to warn him about the possible dangers of doing so. In this smartphone inundated world, I wonder how many people with pacemakers have been affected by this problem. This would be an interesting and timely topic to pursue in further research studies.
I would also like to know how long medical experts have known about the interference cell phones and power lines play in the role of the pacemaker. It seems like something that every patient should be warned about but this is the first I have ever heard of the topic. I plan to do more research on this issue since I have a vested interest in it with my uncle’s health at stake.
Here is the link to the article:
http://www.sciencedaily.com/releases/2015/06/150622071207.htm
Technology, Data and trending
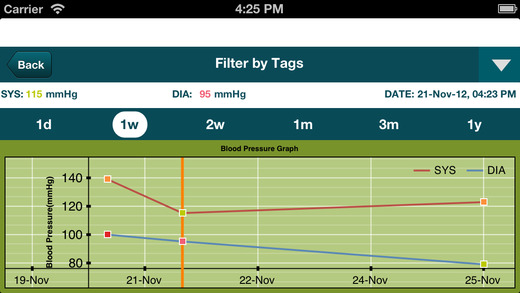
Smart Blood Pressure (SmartBP) BP Tracker

Cardiac Treatment Evolves
Find a webpage, article, or resource focused on newest technology, trends, or procedures related to cardiovascular health. Blog your opinions and thoughts about what you find on your CI Keys page! Be sure to categorize your blog “Goleta420” so it appears in our course Student Blogs page.